Newsroom
The Institute for Health Metrics and Evaluation (IHME) is an independent population health research organization based at the University of Washington School of Medicine.Contact an expert
For media inquiries, please include your deadline in the request and contact [email protected].
IHME in the news
Read what major media outlets are saying about our work.
Insights blog
Find expert insights, commentaries, and researcher explanations of their work.
GBD 2023 Assessment Workshop for Italy
Last updated
March 31, 2025
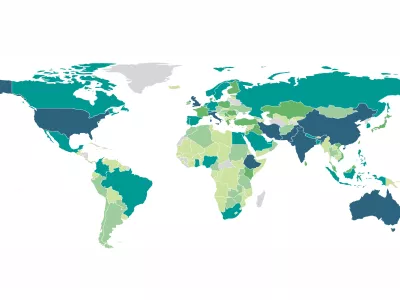
Global Burden of Disease (GBD)
GBD is the single largest and most detailed scientific effort ever conducted to quantify levels and trends in health. It provides a comprehensive picture of mortality and disability across countries, time, age, and sex, incorporating over 350 diseases and injuries in 204 countries.
Videos
Research
Read our peer-reviewed research published in scientific journals.













